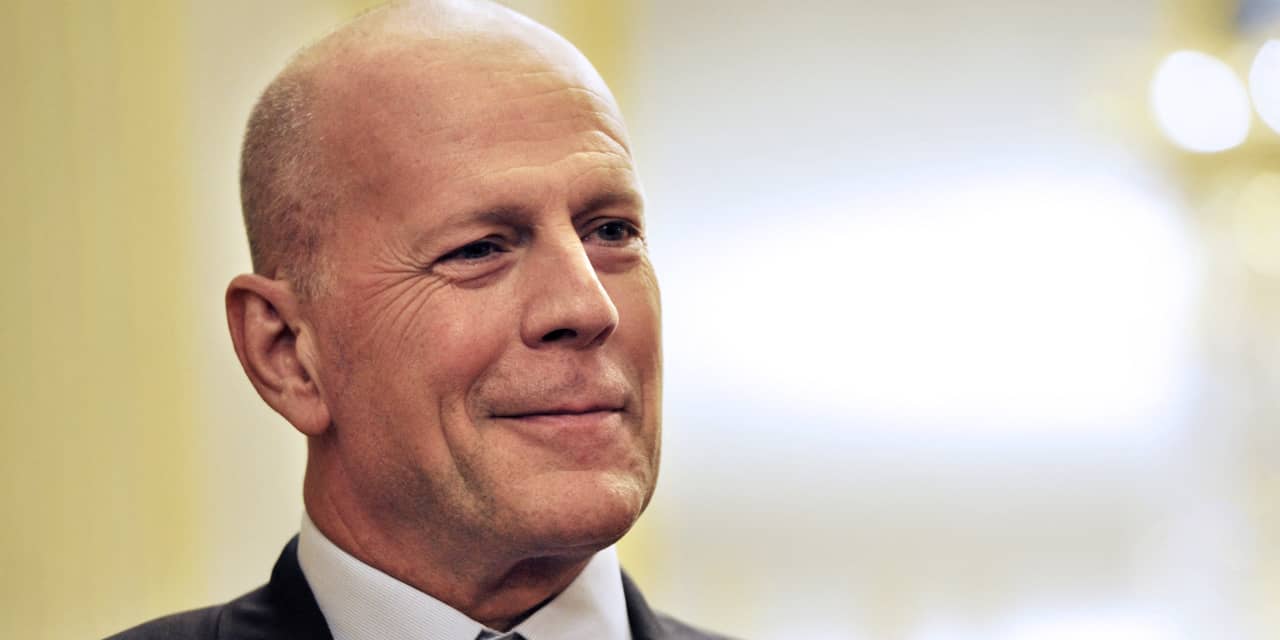
Beloved “Die Hard” and “Moonlighting” actor Bruce Willis has been diagnosed with frontotemporal dementia, or FTD, his family revealed on Thursday, which is the most common form of dementia in people under 60.
“FTD is a cruel disease that many of us have never heard of and can strike anyone,” read the statement signed by Willis’ wife, Emma Heming Willis, his ex-wife Demi Moore, as well as his five children, Rumer, Scout, Tallulah, Mabel and Evelyn.
It was posted to the Association for Frontotemporal Degeneration website, which describes the condition as a group of brain disorders caused by degeneration of the frontal and/or temporal lobes of the brain that often causes personality changes and difficulties communicating. The Association for Frontotemporal Degeneration notes that because most FTD cases occur in people between 45 and 60, who are still in their prime working years, the economic burden of FTD is approximately $120,000 per year, nearly double the amount associated with Alzheimer’s disease.
Related: Bruce Willis is ‘stepping away’ from acting because of aphasia diagnosis
The news led to an outpouring of support for Wills, 67, on social-media sites like Twitter, where his name was trending on Thursday afternoon. But it also raised plenty of questions about what frontotemporal dementia is, and how it differs from Alzheimer’s disease, as well as what Willis’s prognosis could look like.
So here is what we know about FTD so far, including potential causes, signs and resources for those caring for someone with the condition.
What is FTD dementia?
Frontotemporal dementia, or FTD, is also sometimes called frontotemporal lobar degeneration (FTLD), or Pick’s disease. It describes a group of brain disorders caused by the degeneration of the frontal and/or temporal lobes of the brain. And the CDC notes that this type of dementia most often leads to progressive changes in personality, behavior, language and movement because of the part of the brain that it affects.
How common is frontotemporal dementia?
FTD’s estimated U.S. prevalence is around 60,000 cases, but because so many people and health professionals are still unfamiliar with it, it’s hard to say, according to the Association for Frontotemporal Degeneration. FTD is often mistaken for Alzheimer’s disease, for example, or Parkinson’s disease, or depression or a psychiatric condition. So it can take almost four years to get an accurate diagnosis.
What causes FTD? And what are some risk factors?
FTD occurs when abnormal proteins accumulate and clump together in brain cells called neurons, which are the information messengers of the brain that deliver information between different parts of the brain, as well as between the brain and the rest of the nervous system that controls everything you do, such as walking, thinking and feeling. And in some cases, these abnormal proteins accumulate as a result of a change in someone’s genes. But the Association for Frontotemporal Degeneration notes that, plenty of times, the cause of FTD is unknown.
There is evidence to suggest that it can be hereditary, however, with cases reflecting a family history of dementia, a major psychiatric condition, or progressive challenges in movement.
What are some frontotemporal dementia symptoms?
The most common signs of FTD include uncharacteristic personality changes, apathy and unexplained struggles with decision-making, speaking or language comprehension, according to the Association for Frontotemporal Degeneration. The CDC also describes examples like a previously cautious person suddenly saying offensive things and neglecting their responsibilities at home or at work. Or people with frontotemporal dementia may behave inappropriately or embarrass themselves, the CDC cays.
What are the differences between frontotemporal dementia and Alzheimer’s disease?
The Association for Frontotemporal Degeneration points out that while FTD can onset in people between the ages of 21 and 80, it tends to develop much earlier than Alzheimer’s disease does, with most cases occurring between the ages of 45 and 60. It is also less common and less well-known than Alzheimer’s disease. And the Alzheimer’s Association adds that behavior changes are often the first noticeable symptoms of FTD, while these sorts of changes tend to happen later in Alzheimer’s disease. Also, memory loss tends to be a more prominent sign of early Alzheimer’s disease, while this is more common in advanced cases of FTD.
How is FTD treated?
Unfortunately, there are no specific treatments to slow or stop the progression of FTD, although some medications are prescribed to treat depression, agitation and irritability, in order to help improve the patient’s quality of life. Research also suggests that proper nutrition, regular exercise and stress management can also help protect brain function. Caregivers and family members are encouraged to keep people with FTD engaged in activities they enjoy, whether that’s playing cards, birdwatching or whatever they choose. And if these activities become a struggle as FTD progresses, the Association for Frontotemporal Degeneration suggests finding ways to modify the activity. So for example, if someone loves playing poker or bridge, then try playing a more casual or simpler version of the game.
What is the life expectancy of someone with frontotemporal dementia?
So the progression of the FTD symptoms will vary by person, but inevitably there will be a decline in functioning that can vary from two to 20 years, according to the Association for Frontotemporal Degeneration. The person affected will become more vulnerable to to physical complications like pneumonia, infections and injury from falls. The average life expectancy is seven to 13 years after the beginning of symptoms, and the most common cause of death is pneumonia.
There are resources available to help families managing FTD
The Association for Frontotemporal Degeneration (AFTD) has a HelpLine at 866-507-7222, or email info@theaftd.org for guidance and resources regarding your or a loved one’s FTD diagnosis, care and support, as well as opportunities to connect with others in your area.
The Alzheimer’s Association and its 24/7 Helpline at 800-272-3900 has information on Alzheimer’s and other dementias, and can also help you find local support services for FTD.
The Social Security Administration (SSA) at 800-772-1213 has a “compassionate allowance” program where workers diagnosed with Pick’s disease (another name for FTD), PPA or ALS can qualify for Social Security disability benefits.